We use cookies to enhance your browsing experience and analyze the performance of our website. By clicking Continue, you agree to the use of cookies. For more information, please see our Privacy Policy or update your Cookie Preferences.


In this 5-week course, Genova's expert educators break down the science, testing strategies, and treatment protocols you need to address Small Intestinal Bacterial Overgrowth (SIBO) with confidence. [ Save Your Seat! ]

A practical, case-based walk-through of a powerful women's health profile that integrates sex hormones, stress hormones, organic acids, and hormone detoxification insights to inform targeted care.
Michael Chapman, Women's Health+, women's health, womens health, nutrition, overlap
Women's Health+
Dr. Michael Chapman discusses the delicate interplay between sex hormones, stress hormones, and metabolic health in order to bring about a greater awareness of the contribution each has to hormone-mediated cancer risk. He will cover common ways to assess the endocrine pyramid in practice and how to look for imbalances in hormone detoxification to mitigate risk in your patients.
Endo+ Metabolomix+
Most of us clinicians are familiar with the concept of dysbiosis. While this term has been a mainstay of functional GI evaluations for a long time, is it due for an update?
Jeff Bland, Jeffrey Bland, Michael Chapman, Tom Guilliams, Thomas Guilliams
GI Effects
This webinar explores how lab testing can improve patient retention, increase referrals, and support revenue growth - without adding complexity or feeling salesy.
NutrEval GI Effects Metabolomix+
Functional lab testing can feel like a full-time job. Between deciding what to order, analyzing endless reports, and trying to explain the results without overwhelming your patient.
NutrEval GI Effects Metabolomix+
Many practitioners find themselves overwhelmed by complex reports, rushed explanations, and little time to turn insights into action. It's easy for labs to feel like just another task on your plate.
NutrEval GI Effects Metabolomix+
Sleep disruption can quietly drive chronic disease, metabolic dysfunction, and mood disorders. Yet identifying the underlying causes of poor sleep remains one of the most challenging areas in clinical care.
Sleep Assessment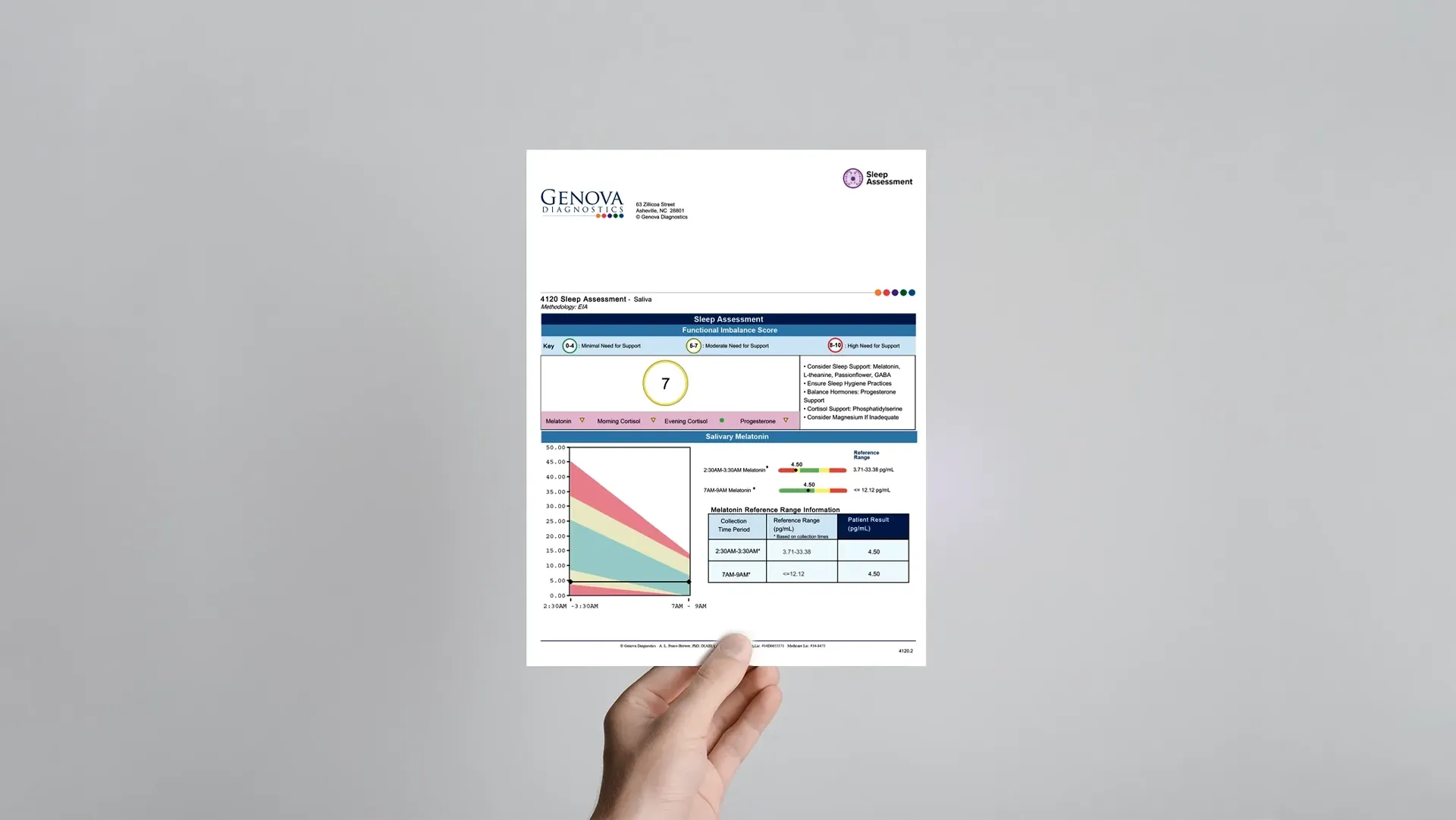
Dr. Michael Chapman will introduce the Sleep Assessment and walk you through how to interpret the report and apply it effectively in clinical workflows.
Michael Chapman
Sleep Assessment
Did you know methylation goes far beyond nutrient SNPs and folate in preconception care? It's a game-changer in fertility and pregnancy health, influencing oogenesis, ovulation, fertilization, and beyond. Please watch our exclusive webinar with Dr. Leah Hechtman, a globally respected naturopathic clinician specialising in fertility, pregnancy, and comprehensive reproductive health.
Methylation
Learn how to design simple programs to address the complex nature of female hormone imbalances.
Endo+
Learn how to correct adrenal lab markers based on supplement protocols and dietary changes, addressing blood sugar and metabolic health.
ASP
Dr. Dale Bredesen and Dr. Kaj Blennow explore one of 2024's most talked-about biomarkers for Alzheimer's diseaseâplasma p-Tau217.
ALzheimer's Assessment
Join Dr. Jeff Bland, Dr. Michael Chapman, and Dr. Christian Jenski as they navigate the Endocrine Maze, and unravel dysfunction for clinical success.
Jeff Bland, Jeffrey Bland, Michael Chapman, Christian Jenski
Endo+
Join Dr. Dan Kalish in partnership with Genova Diagnostics for this free webinar focusing on breast health and assessment of estrogen dominance and estrogen metabolism problems.
Endo+
Join Dr. Dan Kalish in partnership with Genova Diagnostics for this webinar on adrenal treatments that help reset the HPA axis.
ASP
Join Dr. Michael Chapman, Dr. Pam Smith, and Dr. Christopher Mote for an insightful panel discussion moderated by Genova Diagnostics' Cheif Medical Officer, Dr. Patti Smith. This session synthesizes the key concepts from each module of the Unlocking Hormonal Health online course, focusing on holistic strategies, the importance of personalized hormone assessment, and innovative approaches to the neuroendocrine system. Listen in as these distinguished speakers explore the synergies between their methods and share clinical experiences.
Endo+
Dr. Mote specializes in the stress response, circadian rhythm, and sleep optimization for optimal health. Since 2001, he has been teaching on salivary hormone testing, offering unique perspectives on adrenal health assessment. Cortisol serves as a surrogate marker for the body's stress response. He describes the Cortisol Awakening Response (CAR) as âa stress test for the brain and its capacity to organize a stress response.â
Endo+
Explore how stool testing can revolutionize your approach to gut health. This expert-led course is designed for healthcare practitioners eager to deepen their understanding of microbiome health, digestion, absorption, inflammation, and gut function. [ Join the Course! ]

This three-part course with Dr. Laura James equips clinicians to better support patients through the breast cancer journey with integrative, evidence-based strategies. Learn how to strengthen resilience, improve treatment tolerance with nutrition and complementary care, and apply advanced lab testing to reduce side effects, enhance adherence, and promote long-term survivorship. [ Save Your Seat! ]

Hormone assessment can be a complex endeavor for clinicians, given the intricate nature of the hormone cascade and the variety of sample types available for testing. Each patient is unique, emphasizing the need for personalized testing and treatment to efficiently identify and address specific endocrine issues. Root-cause, tailored testing provides an efficient and cost-effective assessment that uncovers each patientâs unique imbalances. In this presentation, Dr. Chapman will provide an overview of current literature on different sample types and the influence of BHRT on testing outcomes. Dr. Chapman will also demonstrate how the Endo+ report can combine various aspects of hormone evaluation to guide personalized treatment plans. Join us to explore common assumptions, emerging trends in hormone research, and the future direction of hormone assessment. Webinar objectives: Develop individualized treatment plans to address hormone imbalance Understand the differences between serum, salivary, and urinary hormone testing Learn to discern which hormone tests best serve each patient's needs Apply best practices and research-backed methodologies to optimize patient outcomes
Michael Chapman
Endo+
Join internationally known physician and author, Dr. Pamela W. Smith, as she introduces the Endo+ profile from Genova Diagnostics. Endo+ sets the standard for comprehensive hormone evaluations, assessing thyroid, adrenal, melatonin, and sex hormones, along with estrogen metabolism. The Endo+ reveals the complex interplay of hormones - not just their levels - providing essential insights for informed treatment and patient understanding. Webinar objectives: Develop individualized treatment plans to address hormone imbalance Understand the differences between serum, salivary, and urinary hormone testing Learn to discern which hormone tests best serve each patient's needs Apply best practices and research-backed methodologies to optimize patient outcomes
Pam Smith
Endo+
A dynamic tour of microbiome management in common gastrointestinal conditions.
GI Effects, stool test, gastrointestinal, microbiome, Joe Feuerstein, Joseph Fuerstein
GI Effects Microbiomix
The GI Effects Comprehensive Stool Profile is a broad assessment of the gastrointestinal tract that offers valuable insight into digestive function, intestinal inflammation, and the intestinal microbiome. Because patient presentations are diverse and complex, it is important to understand both the basics and the subtle nuances when reviewing test results and making therapeutic decisions. So, whether you're new to functional medicine stool testing, or looking to go a bit deeper with your current understanding, this learning module is for you. Join Dr. Christine Stubbe as she uses an actual case study to illustrate how the GI Effects Comprehensive Stool Profile can be used with specific clinical conditions. Learning Objectives Understand the components of the GI Effects Comprehensive Stool Profile Learn how to use the GI Effects with a case study Find out how to access additional learning tools Christine Krall, ND
Christine Krall
GI Effects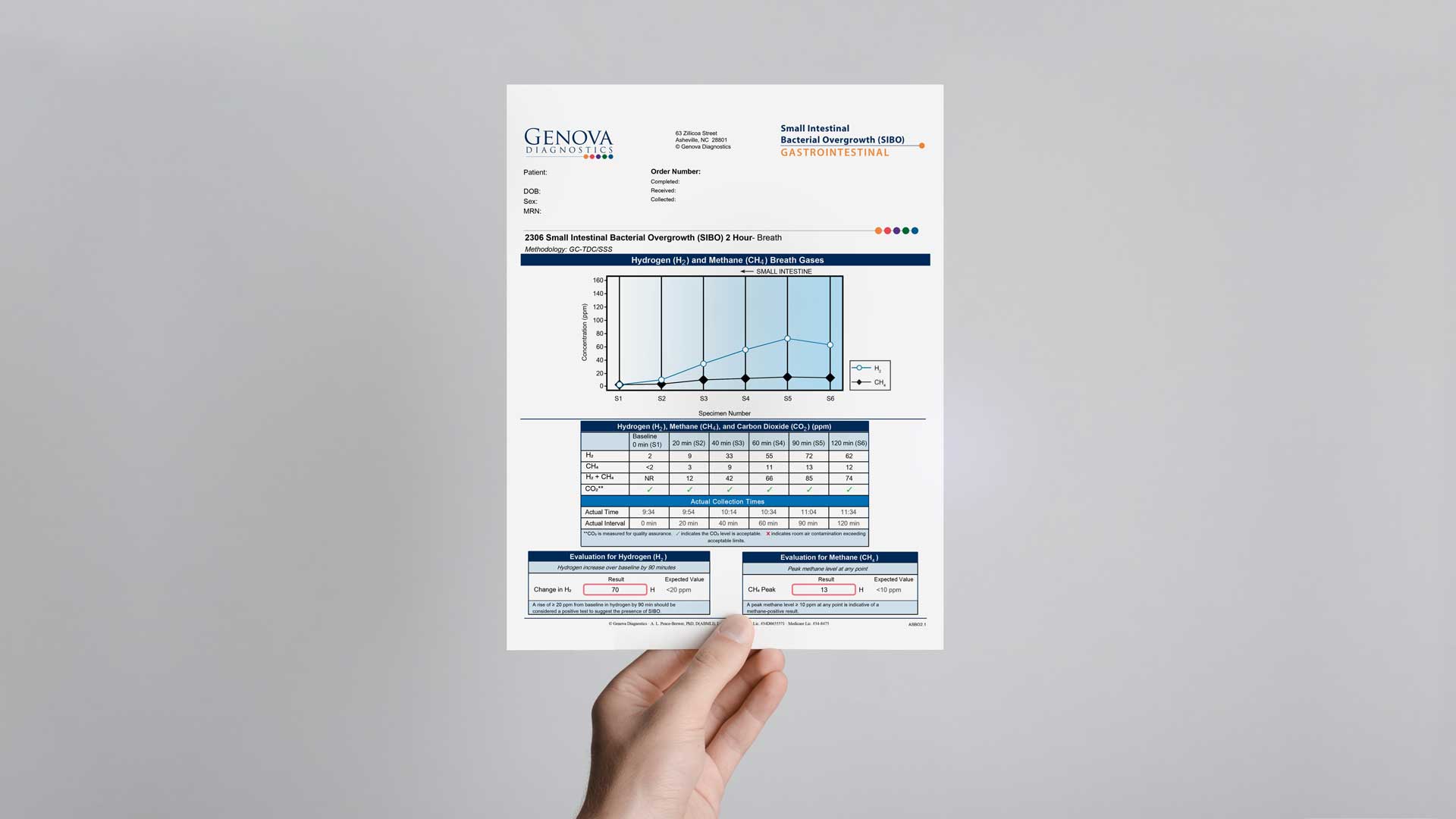
Learn to interpret our Small Intestinal Bacterial Overgrowth (SIBO) breath test with interpretive videos for beginner and advanced users. Each video includes in-depth case study reviews. In this module you will learn how to interpret the SIBO breath test. There is a general overview of the SIBO report itself, followed by a case study. This module is appropriate for a practitioner that is new to Genova's SIBO breath test. This module covers two cases that incorporate testing nuances, such as collecting off schedule, and how to interpret an elevated baseline finding. The patient cases include a patient who has already had SIBO treatment, and another patient who has results from a GI Effects Comprehensive Stool profile with treatment considerations. This module features two patients who had an initial and a follow up SIBO breath test. Testing nuances are discussed, including collecting off schedule and a poor quality sample. These cases highlight the need to treat the underlying cause when follow up tests do not show improvement.
SIBO
The NutrEval, and its subpanels, offer advanced clinical utility to help practitioners identify root causes of dysfunction and treat clinical imbalances that are inhibiting optimal health. The NutrEval is our most comprehensive functional and nutritional assessment including Organic Acids, Oxidative Stress, Amino Acids, Essential and Metabolic Fatty Acids, and Nutrient & Toxic Elements. Customized nutrient recommendations for key vitamins, minerals, amino acids, fatty acids, and digestive support are based on a functional evaluation of important biomarkers. Learning Objectives Learn how to apply the new functional scoring system Understand the interpretation and application of laboratory test results Review therapeutic support options
Michael Chapman
NutrEval
The One Day Hormone Check is a convenient salivary hormone test that evaluates unbound, bioavailable hormone levels over 24 hours. Specimens collected over 24 hours are examined for levels of estradiol, estrone, estriol, progesterone, the progesterone/estradiol ratio (P/E2), testosterone, cortisol, DHEA, and melatonin. The video will help you: Decide when the One Day Hormone Check (ODHC) is the most appropriate profile Interpret the results of the ODHC Place the findings in the context of a case study
One Day Hormone Check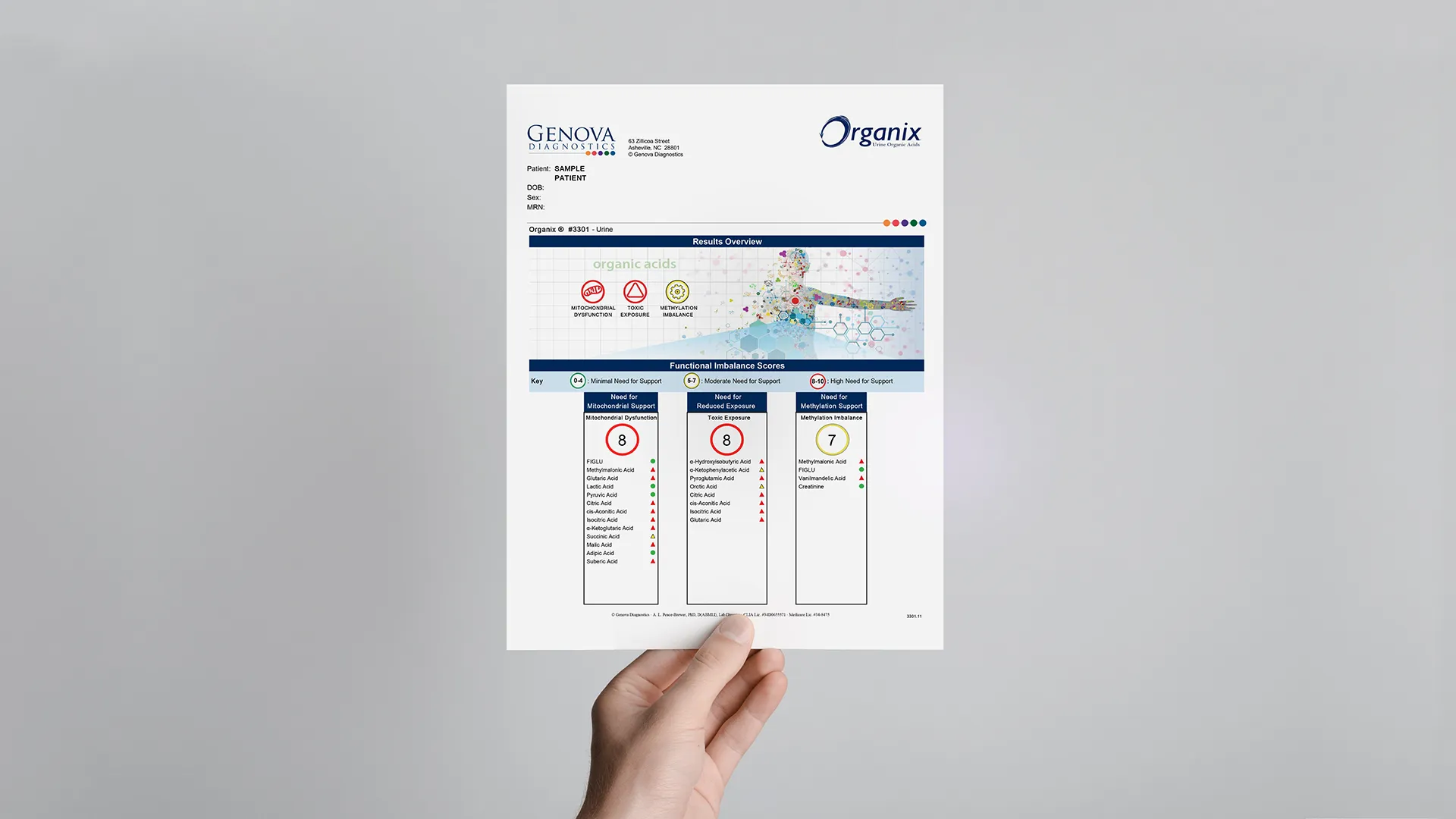
The Organix® Comprehensive Profile is a nutritional test providing insights into organic acids and a view into the body's cellular metabolic processes. Organic acids are metabolic intermediates that are produced in pathways of central energy production, detoxification, neurotransmitter breakdown, or intestinal microbial activity. In this report review video, Michael Chapman will: Help clinicians understand how organic acids may be used to provide unique clinical insight Review the sections of the Organix profile Review therapeutic support options
Michael Chapman
Organix
Microbiomix is a metagenomic stool analysis that assesses a patient's complete gut microbiome as well as its potential function. There are hundreds of species living in the gut with the genomic potential to produce metabolites that promote good health or inflammation and disease. Testing can reveal the balance of these organisms and their potential to produce these metabolites. This metagenomic analysis provides a robust amount of information that has been organized into various sections for ease of use. Dr. Christine Krall gives both a high-level overview as well as digging deeper analysis into the Microbiomix report. Learning Objectives ⢠Learn how to navigate the different sections of the report. ⢠Gain tips for quick assessment. ⢠Understand each metabolite's clinical and therapeutic implications.
Christine Krall
Microbiomix
Join Lahnor Powell as she discusses the potential of the Organix Profile and Organic Acid Testing (OAT). This informative webinar is for everyone, from those seeking health optimization to providers helping patients manage chronic conditions. Discover the role of organic acids in the body and how OAT acts as a personal health blueprint. Lahnor will cover the critical times for OAT, including life-changing events like pregnancy and its importance in regular health assessments. Dive into the key insights OAT provides in Mitochondrial Support, Toxic Exposure, and Methylation Imbalance, enabling you to proactively manage your wellness journey. Learning Objectives Grasp the fundamentals of OAT: its purpose, benefits, optimal timing, and criticality. Identify when OAT is most beneficial, from significant life stages to annual health check-ups. Understand the impact of OAT on Mitochondrial Support, Toxic Exposure, and Methylation Imbalance. Equip yourself with knowledge and confidence for proactive health management.
Organix
Small intestine bacterial overgrowth (SIBO) is a common gastrointestinal disorder that often underlies chronic gastrointestinal symptoms of maldigestion and malabsorption. Assess Patients for SIBO â For in-depth information on our SIBO lactulose breath test, including kit instructions and a sample report, please explore the Small Intestinal Bacterial Overgrowth (SIBO) Breath Test. Presented by Genova Medical Education Specialist, Dr. Christine Stubbe , this information-packed webinar discusses clinically relevant aspects of SIBO diagnosis and treatment.
Christine Krall
SIBOGI Effects
Many of the treatable conditions capable of producing symptoms that meet Rome criteria for IBS can be detected or suggested by evaluation of selected biomarkers that appear in fecal material. Fecal biomarker testing has the advantage of permitting multiple tests, in parallel, on a single specimen. A positive result on one or more fecal biomarker tests may guide therapy, either by suggesting a treatable alternative diagnosis or by eliminating a diagnosis from further consideration, allowing resources to be redirected to more likely diagnoses. Below are links to IBS population studies utilizing Genova stool testing that demonstrate clinical utility and cost-effectiveness. In a retrospective database review study of subjects with IBS-like symptoms, a large proportion (more than 80%) were found to have potentially treatable conditions that produced the IBS-like symptoms. Abnormal values suggesting intestinal dysbiosis, food allergy, parasite infection, exocrine pancreatic insufficiency, or gastrointestinal inflammatory processes were the most common findings.

Uncontrolled and controlled trials in the management of male hormones date back over 70 years. Testosterone replacement therapy for men is safe and can provide significant benefits. This interactive seminar conducted by Dr. Pamela W. Smith, will examine the etiologies of androgen deficiency in males, the signs and symptoms of andropause, testosterone biosynthesis, and review what lab studies to order to effectively manage male hormone replacement. In addition, dosing of all male hormones will be discussed. Key Points: Describe the signs and symptoms of hormone deficiency in a male Understand the functions of testosterone in a male Discuss how to effectively and consistently dose male hormones in men of all ages
Pam Smith
Hormonal Health
"Sportomics" applies metabolomics to investigate the metabolic effects of physical exercise on individuals. "Sportomics" works to advance knowledge in integrative physiology and the systems biology of movement with a goal to translate markers associated with metabolic challenges of training/competition to similar stresses of disease settings. Recent application of microbiome analysis and metabolomics can help further understanding of metabolic health including the benefit of applying movement to chronic metabolic conditions. Microbiome analyses of athletes generally confirm beneficial effects of exercise mechanistically through changes in the gut microbiome. Furthermore, recent developments in microbiome research have highlighted lactate's role in exercise performance and metabolism. Lactate metabolism is tightly regulated and recognized by many as a marker of metabolic health. However, the microbiome utilization of lactate in athletes, specifically by Veillonella atypica, is furthering our understanding of systems biology of metabolic health. Functional medicine testing highlights the changes in exercise metabolomics to guide management and education of patients through movement recommendations. Objectives Use of lactate as a metabolic fitness marker (potential applications of Metabolomix+ to infer areas of education/treatment) Recent studies about the microbiome lactate production/utilization (example(s) from GI effects Jeffrey B. Kreher, MD, FAAP, IFMCPDr.Jeffery Kreher Dr. Jeffrey Kreher, wellstead health's chief medical officer, received his MD from the University of Missouri-Columbia Medical School and did his residency in adult and pediatric medicine at Indiana University, where he served as Chief Resident. He completed a fellowship in Musculoskeletal and Sports Medicine at Boston University/Boston Medical Center, and since 2011, he has practiced sports medicine in the departments of Orthopedics and Pediatrics at Massachusetts General Hospital. Jeff is recognized as a leading educator of patients and health professionals at Harvard Medical School and MGH. His career-long focus has been on providing the highest level of expert, multi-systems care and optimizing the health and well-being of children and adults. Jeff was recently awarded his certification in Functional Medicine through the Institute for Functional Medicine and will shift his practice focus from specialty orthopedic to primary care. Beyond his work life, Jeff's interests include his kids, the outdoors, yoga, cycling, fermenting, philosophy, and board games with his partner, Kirsten.
Nutrition
Learn to analyze Adrenal Stress Profile, improve supplement program design skills, and see how lab results can help you prescribe lifestyle changes.
ASP
No system is more complex or more critical to establishing health than the GI tract. Join Dr. Dan Kalish and Genova Diagnostics for this FREE webinar reviewing clinical treatment models used for generations to restore gut health. This course will introduce you to microbiome analysis and correction of GI issues through interpreting the GI Effects test.
GI Effects
Join Dr. Dan Kalish and Genova Diagnostics for a webinar full of essential patient education tools developed to launch the lab ordering process in your clinic. Specifically designed to educate patients as to the value and purpose of lab tests, these scripts will empower you to order and begin interpreting labs on all your new patients.

Join Dr. Kalish as he discusses how to get started with functional lab testing. You'll learn about the three lab tests to order on every new patient, and the three simple clinical models you can apply to these tests. Dr. Kalish will discuss the adrenal, GI and metabolic testing that he's taught to thousands of practitioners over the past 20 years. This clinical model is in use in clinics worldwide, and has a proven track record of achieving patient results, for both new and seasoned practitioners.
While most of us think of the HPA axis as a "stress" responding system (which it is), we often forget to place the HPA axis into its larger context, that of metabolic regulator. In fact, when we look at the classic HPA axis signaling molecules (i.e., CRH, ACTH, and Cortisol) we find that they regulate a wide range of metabolic functions in both stress and unstressed environments. This webinar will help orient the clinician to a number of other pathways by which the HPA axis functions to modulate and coordinate normal (and stress-induced) metabolism. We will especially focus on the circadian metabolism and show the important connection between the light/dark entrainment of the central clock and the nutrient signals that function at the peripheral clocks. The importance of finding a robust circadian cortisol rhythm (rather than merely the relative levels of cortisol) will be emphasized. Finally, understanding that responding to a metabolic crisis and anticipating a metabolic crisis can elicit the same HPA axis response, help underline the importance of addressing psychosocial stressors in at-risk subjects. Objectives: Reframe the Stress Response within the larger metabolic function of the HPA axis Describe additional components of the HPA axis as key metabolic signals Discuss the function of circadian metabolism as a primary regulator of the HPA axis Define the Responsive and Anticipatory signals that Trigger the HPA axis
ASP
Just like a house is composed of bricks, proteins are made up of smaller building blocks. These building blocks are called amino acids. We consume protein, a macronutrient, from plants and animals which is then broken down into smaller peptides or individual amino acids to be absorbed. Once absorbed, amino acids are used by the body or synthesized into larger proteins. What you can expect: Short discussion covering 5 factors that influence amino acid levels An in-depth dive into a few notable amino acids A brief review of interpreting amino acid intermediary metabolites Lahnor Powell, ND, MPHLahnor Powell, ND, MPH Lahnor Powell, N.D., MPH, received her Doctorate of Naturopathic Medicine from Southwest College of Naturopathic Medicine and her Masters of Public Health from the University of Alabama at Birmingham. Her professional focus is health promotion through community health education and advocacy; dissemination and implementation research; and the science of health innovation. She has contributed to peer reviewed literature and research trials in the field of oncology; mentors adolescents interested in healthcare professions; and competed nationally at the collegiate level in track and field.

The NutrEval, and its subpanels, have been redesigned and reimagined to offer even greater clinical utility! Our nutritional profiles help practitioners identify root causes of dysfunction and treat clinical imbalances that are inhibiting optimal health. The NutrEval is our most comprehensive functional and nutritional assessment including Organic Acids, Oxidative Stress, Amino Acids, Essential and Metabolic Fatty Acids, and Nutrient & Toxic Elements. Customized nutrient recommendations for key vitamins, minerals, amino acids, fatty acids, and digestive support are based on a functional evaluation of important biomarkers. New product line features include: Functional pillars with a built-in scoring system to guide therapy around needs for methylation support, toxic exposures, mitochondrial dysfunction, fatty acid imbalances, and oxidative stress Dynamic biochemical pathway charts to provide a clear understanding of how specific markers play a role in biochemistry Updated Interpretation-At-A-Glance pages providing educational information on nutrient function, causes and complications of deficiencies, and dietary sources Michael Chapman, NDLahnor Powell, ND, MPH Michael Chapman, N.D., is a licensed naturopathic physician who graduated from Bastyr University in Seattle, Washington. Upon graduation, he spent three years in private practice before joining the team at Genova Diagnostics. His areas of clinical focus are hormone regulation, gastrointestinal health, and autonomic balance. Prior to medical school, Dr. Chapman earned his Bachelor of Science degree from Indiana University with a focus in neuropsychology. He later worked as a microbiologist performing pharmaceutical research on cancer cell lines. Dr. Chapman has a passion for learning and helping others come to a greater understanding of the vast and dynamic processes that exist and interact within the human body.
Michael Chapman
NutrEval
Infertility is increasing, along with the use of reproductive technology. One of the most overlooked and undervalued approaches to fertility is screening the couple's preconception health and evaluating nutrition. Ideally, 3-6 months months prior to conception, we would want to optimize nutrient reserves, decrease toxic burden, and promote a healthy diet. In other words, prepare a healthy seed and healthy soil. With the use of functional medicine nutrition testing, we are able to directly get an assessment of several nutrients-including fatty acids, B-vitamins, and minerals-that has been shown to help optimize fertility health and lead to better pregnancy outcomes. Join nurse practitioner Taylor Dukes in discussing a preconception protocol to optimize egg quality. Learning Objectives Understand how to optimize body prior to conception Review of macro and micronutrients to support conception and pregnancy Using the NutrEval and Metabolomix+ profiles, discuss common nutrient deficiencies important for conception Taylor Dukes, FNP
NutrEval
The popularity of dietary supplementation continues to grow. It is the foundation of the health-promoting strategies of thousands of healthcare professionals and millions of Americans. Yet, clinicians and patients are routinely faced with an onslaught of confusing, contradictory, over-hyped, and often misleading information about nutrition - especially dietary supplementation. Are "natural" supplement ingredients always better, or even different, than "synthetics?" Are mineral chelates always a better choice than ionic salts? Are there real differences between various types of fish oils? What are "whole food" supplements and are they really what they claim to be? Are "activated" B-vitamins necessary and superior to other forms of B-vitamins? This webinar will cut through these issues and help answer real-world questions regarding supplementing dietary nutrients within the context of clinical practice. Learning Objectives: Help clinicians understand practical differences between "natural" and "synthetic" vitamin compounds and distinguish when those differences matter clinically Clear up confusion about many marketing terms used to promote vitamins that are often false or misleading Discuss why some bioavailability changes of nutrients (including phytonutrients) alter their efficacy, while others do not Thomas G. Guilliams, Ph.D.

The Lab Report is Genova's fun-filled podcast about all things functional medicine, laboratory testing, and integrative therapeutics. It is cohosted by our Medical Affairs team members Dr. Michael Chapman and Dr. Patti Devers. The show is light-hearted, but also jam-packed with clinical information. The Lab Report has garnered some impressive feedback in the functional medicine space and its fan base continues to grow. From lab testing, to physiology, to interviews with some very high-profile guests, this Genova podcast is perfect for clinicians new to functional medicine or those looking for deeper insight. This month, The Lab Report visits LiveGDX. The tables are turned as we interview the interviewers. Patti & Michael talk about their favorite moments from the podcast and discuss some fun clinical pearls relating to our flagship products, the NutrEval and GI Effects. Clinical Pearls: Medication and Supplements; Interferences vs. Influences When Biomarker Sensitivity and Specificity are appropriate Culture vs. PCR for Yeast/Mycology Evaluation Functional vs. Direct Nutritional Assessments Urine vs. Blood for Evaluating Toxic Exposures Michael Chapman, ND Patricia Devers, DO
Patti Devers, Patricia Devers, Michael Chapman

DNA methylation plays a central, potentially lasting, (and heritable) regulatory role in health and disease. Aberrant methylation patterns, resulting in regions of hyper- and hypomethylation, influence the course of most, if not all, chronic disease. In cancer, it is understood that epimutations outpace genetic mutations 10:1. It's also understood that lifestyle factors can profoundly influence epigenetic methylation expression. Integrative and Functional Medicine clinicians, in employing a systems approach to care, are arguably best suited to optimize their patient's genetic expression. Learning Objectives: Review DNA methylation and its importance to aging and healthspan Discuss the wide range of factors that influence methylation status Provide practical assessment and intervention tools to support balanced methylation, including supplements, diet, and lifestyle Learn what's next in assessing the methylome in clinical practice Kara Fitzgerald, ND
Methylation
Methylation is a complex process in which methyl groups (CH3) are transferred or donated between molecules, thereby changing their structure and function. This happens billions of times per second in every cell throughout the body. The methylation cycle is dependent on amino acids, vitamin cofactors, and minerals obtained from the diet to facilitate adequate function of this complex biochemical pathway. Proper methylation is crucial to an enormous number of systemic biological processes, including creatine production for skeletal muscle contraction, DNA and RNA synthesis, gene regulation (epigenetics), hormone regulation and detoxification, energy production, cell membrane repair, fat metabolism, myelination, and immune function. However, key amino acid deficiencies, lack of vitamin and mineral cofactors, genetic enzymatic predispositions, and a wide array of oxidative stressors can affect each of these pathways and a patient's overall methylation status. The webinar will introduce the innovative Methylation Panel, offering insight into the critical biochemical methylation pathway. By measuring analytes involved in the methylation cycle, as well as testing genetic predispositions for altered enzymatic activity, this profile can help clinicians design more targeted treatment strategies to optimize patient outcomes. Learning Objectives: Review the methylation and transsulfuration pathways Discuss the interpretation and application of laboratory test results Apply nutritional and lifestyle therapies to support methylation status Michael Chapman, ND
Michael Chapman
Methylation
Alzheimer's disease represents a major healthcare crisis. An estimated 5.7 million Americans suffer from this disease. As the most common type of dementia, Alzheimer's disease is a neurodegenerative disease characterized by the presence of beta-amyloid and tau proteins within brain and nerve cells. This condition disproportionately impacts menopausal women to the tune of 3.2 million diagnosed with this condition. A few unmodifiable risk factors have been identified, such as aging, family history, and genetics, but we are only beginning to understand the link between different hormones and Alzheimer's, particularly in menopausal women. Epidemiological studies highlight metabolic abnormalities as an important contributor to Alzheimer's disease. Thus, early and accurate identification of metabolic risk factors, such as insulin resistance and hormonal imbalances, may help to delay or decrease progression of Alzheimer's disease. Doctor Trindade will discuss her unique approach, which incorporates functional medicine principles, and offer clinical pearls to address Alzheimer's disease, particularly in women. This webinar will focus on applying and interpreting treatable metabolic and hormonal abnormalities, shown in research to be contributing risk factors for the development and progression of Alzheimer's disease. Learning Objectives: Describe the contribution of insulin resistance and hormonal imbalance in the development and progression of Alzheimer's disease Review a treatment approach in patients with increased risk, or who already have, Alzheimer disease Filomena Trindade, MD
filomena trindade
Hormones play a critical role in maintaining optimal health. The proper balance of estrogen, progesterone, and testosterone are essential for muscle and skin tone, bone resilience, libido, fertility, weight management, energy levels, and a healthy menstrual cycle. Imbalanced hormones affect sleep, metabolic rate, and immune system function, and contribute to the development of osteoporosis, breast and endometrial cancer, and heart disease. The Rhythm Plus hormone test is a comprehensive salivary assessment of estradiol, progesterone, and testosterone that spans a full 28 days. Additionally, this hormone testing profile includes the Adrenocortex Stress Profile and the Comprehensive Melatonin Profile to reveal how the sex hormones are influenced by cortisol, DHEA, and melatonin. Rhythm Plus is a hormonal test indicated for both premenopausal and perimenopausal women not currently supplementing with hormones. Learning Objectives Assess the menstrual cycle utilizing salivary hormones Review the components of the Rhythm Plus Profile Discuss HPA axis insights provided by cortisol and melatonin circadian rhythms Apply test results to patient scenarios using case studies Stephen Goldman, DC
Rhythm Plus
Small intestine bacterial overgrowth, or SIBO, is a condition in which the small bowel is colonized by microbes normally found in the large intestine. This common gastrointestinal disorder is characterized by maldigestion and malabsorption of critical nutrients. SIBO presents with IBS-like symptoms (i.e. abdominal bloating and gas, changes in bowel habits, abdominal pain, nausea and vomiting) which are intensified postprandially. The gold standard of SIBO diagnosis is small bowel fluid aspiration followed by culture. Due to the invasive nature of this procedure and the many shortcomings, assessing breath gases following a challenge drink has been widely accepted. Due to the increasing literature and medical attention, new SIBO guidelines have been established for clinicians and researchers to help standardize testing and interpretation of results. In this webinar, Dr. Stubbe will review the new SIBO guidelines and discuss the latest option of a 2- and 3-hour breath test offered at Genova Diagnostics. In addition, interventions involving diet, digestive support, probiotics, and antimicrobials will be discussed. In this webinar you will learn: Common underlying causes of SIBO Current guidelines as it relates to testing and interpretation of the SIBO breath test Interventions used to treat and prevent SIBO Christine Stubbe Krall, ND
Christine Krall
SIBO
Are You Tired of Being Tired? Cortisol is the body's main stress hormone and is released in a natural diurnal circadian pattern under ideal circumstances. However, as we face many different daily stressors additional cortisol release is provoked. Repeated activation of this "fight or flight" response can lead to HPA axis disruption and dysregulation. In addition to cortisol's circadian rhythm, there is a separate and distinct transient increase in cortisol triggered merely by the act of waking in the morning. This is called the "Cortisol Awakening Response" or CAR. This response offers additional insight into the resiliency of the HPA axis and has distinct health implications. Assessing cortisol using both CAR and the diurnal rhythm helps to identify abnormalities and allows clinicians to address root causes. Objectives Review of the HPA axis Define what CAR is and how it is related to HPA axis Use case review to discuss what to do with an altered CAR Filomena Trindade, MD MPH
filomena trindade

In this session, Dr. Wahls will discuss the use of diet to treat Multiple Sclerosis (MS) related symptoms. She uses diet and lifestyle interventions based upon Functional Medicine and Ancestral Health principles to treat a wide variety of neurological, medical and psychiatric disorders. In addition, she conducts clinical trials using diet and lifestyle to treat multiple sclerosis. Dr. Wahls has a personal connection to these interventions, having experienced 7 years of steady decline due to progressive MS, and even spent four years dependent upon a tilt recline wheelchair. Thanks to the power of functional medicine, diet and lifestyle interventions she restored her health and vitality, and now bikes to work. She will review her personal story, the scientific rationale for her treatment protocols, and provide updates from her clinical research into the use of diet and lifestyle to treat progressive and relapsing-remitting MS. Learning Objectives: Understand the mechanisms by which dietary factors may contribute to neuroinflammation, neurodegenerative disease, and potential worsening of MS related symptoms Learn specific food groups that can help stabilize and/or reverse neurological disease processes and MS related symptoms Identify an effective test that clinicians can use to monitor the microbiome Identify testing to guide supplementation strategies for MS patients Multiple Sclerosis food diet and lifestyle lifestyle interventions Terry Wahls, MD
While there is much discussion about "Leaky Gut Syndrome" within the integrative medical community, there is less knowledge about the fundamentals of the gut barrier and how the microbiome and immune system function to maintain that barrier. This lecture is designed to bring clinicians "up-to-speed" on the basic fundamentals of gut barrier physiology, discuss the primary ways that it fails (and how to test for this) and review the evidence for non-pharmacological therapies that can improve gut barrier function. Learning Objectives: Understand the cells, proteins and processes that are designed to maintain a healthy gut interface. Understand how the microbiome and immune system interface, and is dependent on a close, but controlled interface through the gut epithelial layer. Review tests and clinical signs used to assess the functional permeability of a person's gut barrier. Learn the evidence for specific therapies that can improve barrier function Keywords: gastrointestinal disorders intestinal barrier function Leaky Gut Syndrome Thomas Guilliams, PhD
GI Effects
Are you doing all you can to assess your patient's individual risk for a hormone-related cancer, such as breast cancer in women and prostate cancer in men? Estrogen-metabolism assessment should be an essential part of a comprehensive preventive or functional health program, regardless of whether the patient is male or female. Each patient's individual differences, including genetic as well as environmental factors, can affect potential risk. Optimizing estrogen metabolism includes supporting both phase 1 and phase 2 detoxification pathways, with particular attention to single nucleotide polymorphisms (SNPs) that may be present. In addition, xenoestrogens and toxin exposure will affect the metabolism of estrogen. The literature supports using estrogen metabolism assessment and optimization as part of a cancer prevention program. Are you doing all you can to assess your patient's individual risk? If not, join us for this informative LIVEGDX presentation. Learning Objectives Discuss the role of estrogen metabolism in the evaluation of hormone-related cancer risk Learn what environmental and lifestyle factors may affect estrogen detoxification Introduce therapeutic options focusing on improved estrogen metabolism Keywords: estrogen metabolism breast cancer prostate cancer Filomena Trindade, MD MPH
filomena trindade

Women struggling with any chronic illness naturally want the fastest route to wellness, and that's what practitioners want to provide. Whether for ourselves or our clients, we need to take a deep look at what the body is trying to say and answer that call in our healing strategy. Adrenal dysregulation and "the-survival-mode" root cause of Hashimoto's are examples of how self-preservation can lead to systemic imbalance, and how the wound reveals the cure. In this one-hour webinar, Dr. Romm will provide a unique and even counterintuitive approach to help women restore their energy, immunity, and take back their lives. From Dr Romm's insights, you will take away new strategies that will help patients not just overcome symptoms, but truly heal the body and restore quality of life through replenishment. Explore the connection between metabolism, hormones, mind, and mood Discuss root causes of dysfunction as they relate to lifestyles in "survival mode" Learn strategies for addressing adrenal and thyroid imbalances Keywords: adrenal dysfunction thyroid dysfunction autoimmune Aviva Romm, MD
ASP
This presentation will take detoxification to the next level of science and clinical application. You will learn how to apply your patient detoxigenomic SNP results into a personalized plan encompassing diet and lifestyle strategies. There will be particular focus on nutrition, nutrient actives, and botanicals for their influence on detoxification pathways. Additionally, incorporation of lifestyle changes will be included as part of the detox discussion for a more well-rounded, whole picture, whole-self approach to detoxification. Learning Objectives: To understand the latest science on diet and lifestyle for clinical applications to detoxification concerns To learn how to apply diet and lifestyle to phase I and phase II detoxification SNPs To understand the steps of how to compose a personalized plan for patients who need to detoxification Keywords: detox genomics personalized medicine Deanna Minich, PhD
DetoxiGenomic Profile
Food sensitivities have been associated with a wide range of medical conditions affecting multiple body systems. Using an effective case-study approach, Dr. Kathleen O'Neil-Smith presents a detailed discussion of IgG/IgE testing and the application of therapeutic treatment plans. Dr. O'Neil-Smith will demonstrate how to use testing to evaluate a patient's total antigenic load with regard to food and environmental sensitivities and the clinical use of elimination diets. Learning Objectives: Become familiar with IgG-mediated food testing and the indications for ordering an IgG food-antibody test Review case histories and discuss how to use elimination diets in clinical practice to help patients with IBS, post-infectious IBS, and other related conditions Explore additional testing that assists the clinician in addressing GI health and healing Keywords: GI health Food sensitivities elimination diet Kathleen O'Neil-Smith
Food Sensitivity+
The human intestinal microbiota functions as an organ and is critical for immune and gastrointestinal system maturation, colonization resistance, modulation of immune responses, and nutritional needs. A balanced, diverse microbiota is essential for health. There are disorders in which the beneficial use of probiotics is documented including antibiotic-associated diarrhea, C. difficile-associated diarrhea, inflammatory bowel disease, irritable bowel disease, dysbiosis, urinary tract infections, allergies, atopic dermatitis, eczema, and lactose intolerance. As a complementary therapy, prebiotics increase the numbers and/or activities of healthful gut microbiota and support populations of healthful genera that are not available as probiotics. This presentation will provide the knowledge and tools needed to effectively use prebiotics and probiotics to enhance health. Learning objectives: Understand the beneficial effects of the gastrointestinal microbiota on the development and function of the immune, gastrointestinal, and other organ systems, as well as the adverse effects that can occur secondary to microbiome disruption Appreciate the mechanisms by which probiotics may confer benefit and the health conditions for which evidence exists to support their use Learn the safety profile and potential risks of probiotic preparations and how to effectively select and dose probiotic formulas Keywords: weight management hormonal imbalance nutritional insufficiences Stephen Olmstead, MD
GI Effects
A good night's sleep, while fundamental to maintaining health, is not sufficient to prevent the ill effects of the sustained physical and psychological stress that many of our women patients face. The frequent activation of the body's stress response leads to a state of chronic hypervigilance, unleashing a cascade of stress hormones and other stress-mediating physiological agents that can lead to a host of health conditions â metabolic syndrome, reproductive disorders, chronic fatigue syndrome, autoimmune disorders, and many others. The adaptogens are an important therapeutic category of botanicals that can reduce not only stress-related symptoms, but prevent or mitigate the long-term effects of stress on the body, thus reducing our allostatic load. They are used to promote a sense of well-being, improve energy and stamina, reduce fatigue, improve immunity, and enhance mental concentration, and promote hormonal balance due to their regulating effects on the HPA axis. In so doing they aid the body's innate ability, when thrown off by stressors, to recover homeostatic balance or homeostasis. Learning Objectives: Review the impact of HPA axis dysregulation on women's health Understand the concept of adaptogens Discuss 5 common botanical adaptogens, their applications, safety, and potential herb-drug interactions Keywords: women's health adaptogens stress Aviva Romm, MD
ASP
Dr. Smith is a recognized Anti-Aging and Metabolic Medicine Specialist and uses bioidentical hormone therapy extensively in her practice. Join Dr. Michael Chapman as he interviews Dr. Smith about normal hormone production in both men and women, the consequences of hormonal imbalance, and the importance of laboratory testing as an essential tool for personalizing hormone therapy and achieving effective clinical results. Learning Objectives Learn the significance of steroidogenic pathways How to start using hormone therapy Understand the importance for balance Learn how to apply Therapeutic Ranges in your clinical practice Pamela W. Smith, MD, MPH, MS
Pam Smith
Clinical Pearls
Case history presentations are effective in illustrating the process of applying therapeutic ranges in treatment. In this webinar, Dr Pamela W. Smith will review case histories to assist the clinician in better understanding the clinical relevance of therapeutic ranges for the sex hormones, including estrogen, progesterone, and testosterone, plus the adrenal hormone, DHEA. Dr. Smith will discuss how to approach dosages for menopausal women on natural prescription hormone therapy. Emphasis will be placed on new treatment modalities relating to adrenal dysfunction in order to cultivate a better understanding of the interplay and balance between adrenal hormones and sex steroid hormones. Webinar objectives: Learn the average amount of estrogen, progesterone, testosterone, and DHEA that women make naturally Review case histories and discuss prescribing techniques for menopausal hormone therapies Examine the importance of hormonal balance between sex hormones and adrenal hormones Keywords: bio-identical hormone therapy hormone balance hormone case studies
Pam Smith, Pamela Smith
The HPA axis is the body's stress response system. Acute stress causes the HPA axis to start a systemic hormonal cascade that enables the body to react quickly to the stressor - the "fight or flight" response. In today's world, stress is often chronic, but the HPA axis responds in the same way as it does to acute stress. This results in a repetitive and continuous stress hormone cascade that impacts every system in the body. Patients who experience this constant sympathetic state have a variety of symptoms that can be vague and seemingly unrelated. In this webinar, Dr. Michelle Maddux uses case studies to illustrate how adrenal dysfunction and GI conditions may be related, and discusses how to assess and treat complex patients with GI complaints. Clinical Pearl 1 When a patient has multiple symptoms in several systems that are fundamental to health, where do you begin to sort it out? In this segment, Dr. Michelle Maddux describes an approach that can be used in complex patients. The Cortisol Awakening Response (CAR) and the cortisol diurnal curve tell us different things about the HPA axis function and dysfunction. Listen as Dr. Michelle Maddux explains the difference between the two patterns and mechanisms, and what they can tell us about underlying problems and root causes. To accurately measure CAR, the timing of sample collection is critical because the response is transient. Here Dr. Michelle Maddux answers the most common questions about sample timing, including the definition of "awake."
Clinical Pearls
What do premenstrual syndrome (PMS), polycystic ovary syndrome (PCOS), and many cases of infertility have in common? As Dr. Pamela W. Smith states on these conditions, "It's all about hormone balance. Balance is the key." Estrogen, progesterone, testosterone, cortisol, thyroid, melatoninâin fact, all the body's hormones are interconnected in a delicately balanced dance. For many menstruating women, however, this dance can sometimes lose its rhythm, resulting in the altered production of one hormone, leading to the altered production of another, and perhaps another⦠These hormone imbalances can be the root cause of a wide-array of symptoms, seemingly unconnected, which often makes diagnosis of the underlying problem a frustrating experience for the patient and the healthcare provider. Dr. Smith has found that three of the most common conditions related to imbalanced hormones are PMS, PCOS, and infertility: PMS - the great masqueraderâfrequently misdiagnosed as a psychological problem and causing symptoms as diverse as acne, asthma, backache, bleeding gums, clumsiness, confusion, cravings, cramps, dizziness, migraines, mood swings, poor judgment, visual changes, tingling, or tremors PCOS - affecting nearly 10% of women in America and accounting for 85% of women with androgen excess and increased growth of facial and body hair; produces infertility in 75% of obese women who have PCOS, and can be associated with increased risk for diabetes, lipid abnormalities, and cardiovascular disease The value of salivary hormone testing - how testing hormone levels over a 28-day cycle yields vital clinical clues to a women's individual "hormone dance" and provides guidelines for the development of personalized treatments Effective natural therapies - that can produce profound effects on hormonal balance including dietary composition and timing, nutrients and botanicals that can help (or harm), and lifestyle interventions to minimize toxic exposure and reduce stress
Pam Smith, Pamela Smith
Rhythm Plus
Download PDF
GI Effects, stool test, gastrointestinal, microbiome, dysbiosis, pathogens, H. pylori, parasites, commensal bacteria, calprotectin, lactoferrin, secretory IgA, pancreatic elastase, steatocrit, short-chain fatty acids, butyrate, beta-glucuronidase, maldigestion, inflammation, leaky gut, IBS, IBD, SIBO, FIT, PCR, antibiotic stewardship
Support Guide: Hormonal Health
Download PDF
sex hormones, estradiol (E2), estrone (E1), progesterone, testosterone, free testosterone, DHEA-S, SHBG, LH, FSH, prolactin, cycle day 3, luteal phase, perimenopause, menopause, PMS, PCOS, androgen excess, estrogen dominance, adrenal-ovarian balance, infertility, men's health, women's health, hormone optimization

Download PDF
NutrEval, micronutrient testing, organic acids, OAT, mitochondria, methylation, MTHFR, B-vitamins, CoQ10, carnitine, amino acids, fatty acids, omega-3 index, oxidative stress, glutathione, dysbiosis markers, minerals, toxic elements, nutrient deficiencies, metabolic pathways, energy production, functional nutrition